A new clinical trial for the treatment of Chagas disease has shown that the low-dose drug fexinidazole is well tolerated by patients, but is not effective in sustainably eliminating the Trypanosoma cruzi parasite, responsible for causing the disease. The results have just been published in the scientific journal The Lancet Infectious Diseases.
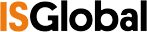
The FEXI-12 study, funded by DNDi and coordinated by the Barcelona Institute for Global Health (ISGlobal), a centre supported by the "la Caixa" Foundation, was conducted in five hospitals in Spain with extensive experience in the care of patients with Chagas disease. Fexinidazole was shown to be effective in an earlier clinical trial that was stopped because the doses tested were not well tolerated. The new phase 2 trial evaluated fexinidazole at lower doses and with a shorter duration of treatment. In total, three fexinidazole regimens with different durations and doses were evaluated. Although the volunteers tolerated all the regimens tested and the parasite load decreased significantly after treatment, a rebound effect was observed ten weeks later. The research team therefore decided to discontinue the development of fexinidazole as a monotherapy for the treatment of Chagas disease.
"Despite its good tolerability, fexinidazole does not show sufficient efficacy against the T. cruzi parasite and is therefore not a viable alternative for the treatment of Chagas disease," says Julio A. Padilla, director of ISGlobal's Chagas Initiative. "The search for alternatives, whether new products or the recovery of compounds used in other diseases, is a priority. To this end, ISGlobal is participating in the TESEO study with the aim of optimising the current regimens of the drugs currently used (benznidazole and nifurtimox), while investigating potential biomarkers of therapeutic response".
Chagas, a neglected disease
Chagas disease is a neglected disease. It is estimated that less than 1% of patients have access to treatment with benznidazole or nifurtimox. Both drugs were developed more than 50 years ago and frequent side effects associated with their use are a major barrier to treatment, causing one in five patients to discontinue treatment. In several clinical trials, standard treatment with benznidazole has been shown to be effective against infection with a sustained effect for at least 12 months after treatment in about 80% of treated patients. Optimisation of existing treatments through the use of alternative regimens remains a promising line of research.
Shorter treatments for Chagas disease
"At DNDi, we are working with partners on the NuestroBen study, which aims to assess whether a shorter benznidazole regimen has the potential to become the standard for treating Chagas disease. We hope that a shorter treatment duration will improve the risk-benefit ratio of the drug and increase adherence. Making available therapies simpler and safer is a potentially faster way to improve the quality of life of those affected, while we advance the longer process of molecule research to find a completely new drug for Chagas disease," says María-Jesús Pinazo, head of DNDi's Chagas disease programme.
Following the completion of the BENDITA trial, which suggested that a shorter duration of benznidazole treatment could maintain high antiparasitic efficacy, new trials are underway. These trials aim to provide clearer evidence on the feasibility of alternative regimens to current drugs, and whether these can improve tolerability and adherence while reducing the incidence of adverse effects. Meanwhile, drug discovery efforts continue, with promising new chemical entities entering phase 1 and 2 trials.
Reference
Pinazo MJ, Forsyth C, Losada I, Trigo Esteban E, García-Rodríguez M, et al, on behalf of the FEXI-12 Study Team. Efficacy and safety of fexinidazole for treatment of chronic indeterminate Chagas disease (FEXI-12): a multicentre, randomised, double-blind, phase 2 trial. Lancet Infectious Diseases. 2024. https://doi.org/10.1016/S1473-3099(23)00651-5