Brain Alterations Detected in Obese Children
The alterations link obesity to a brain condition similar to obsessive–compulsive disorder, which affects the same areas of the brain
09.06.2021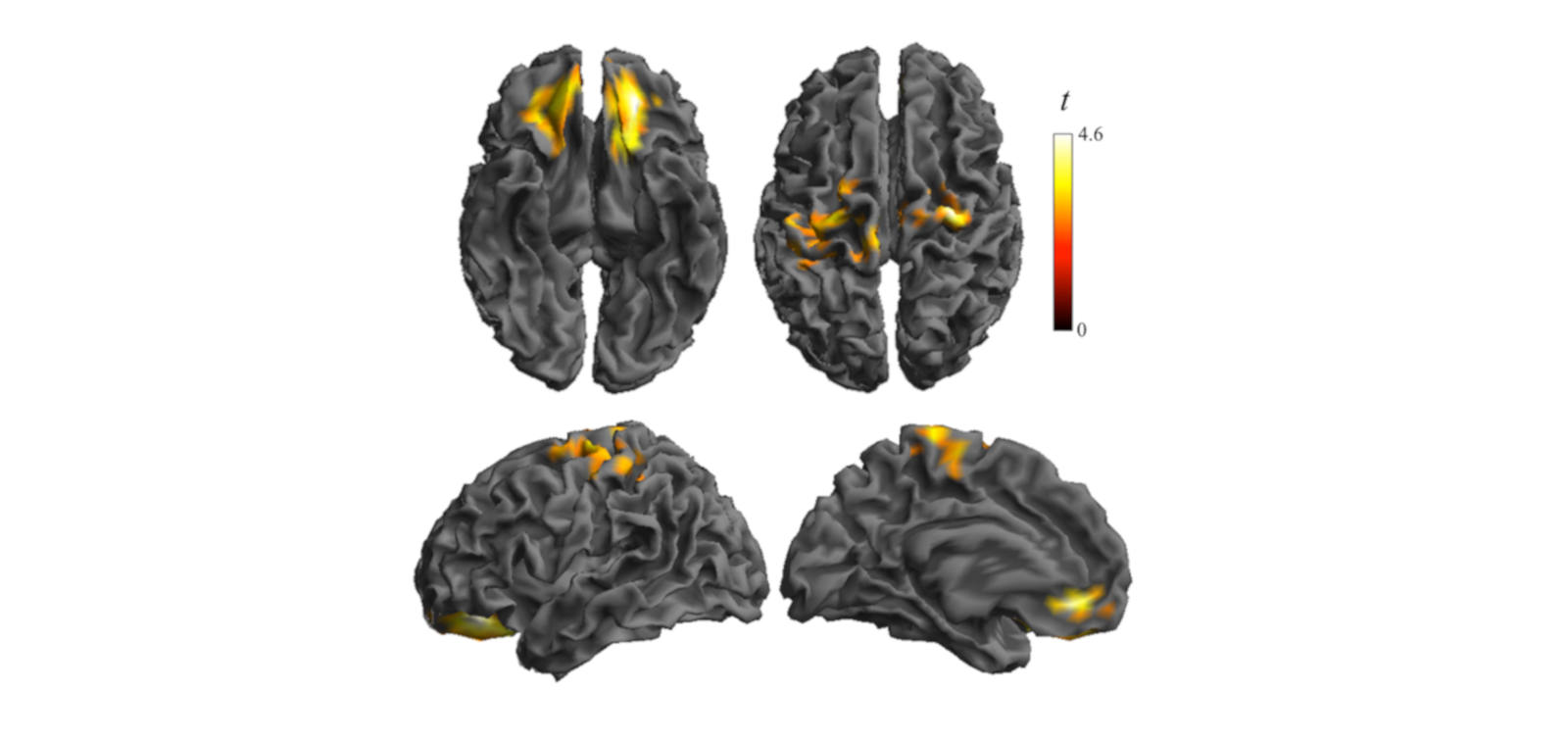
Obesity is generally linked to poor eating habits and the availability of tasty, high-calorie foods. However, a new study led by researchers from the Magnetic Resonance Imaging Research Unit in the Department of Radiology at Hospital del Mar and the Barcelona Institute for Global Health (ISGlobal), a centre supported by the ”la Caixa” Foundation, has found that more elements are involved. Thanks to images obtained by functional magnetic resonance imaging, the researchers found that certain parts of the brains of obese children show alterations with respect to normal-weight or overweight children of the same age. The study findings were published in the journal Cerebral Cortex.
“Obesity in general, and childhood obesity in particular, is seen as a bad habit and certain foods are blamed for it, but this is not entirely true,” commented Dr. Jesús Pujol, co-author of the study and head of the Magnetic Resonance Imaging Research Unit. The study, he explained, found “a qualitative leap, in which what is viewed as a bad habit in overweight children becomes a brain ‘disease’ in the form of functional alterations when overweight becomes obesity. It is clearly an obsession with food.”
A brain unlike that of normal-weight and overweight children
The brains of obese children were found to have different features from those of normal-weight or overweight children. The researchers analysed images of the brains of 230 children aged 8-12 years (volunteers in the BREATHE study led by ISGlobal) using techniques developed by the Hospital del Mar team and determined that two areas of the brain were altered and hyperexcited. The affected regions were the orbitofrontal cortex and the amygdala, the centres that regulate reward and punishment sensations and their relationship to the part of the brain that regulates basic needs, such as food and emotions, and the somatosensory cortex, where the brain represents body image. The study is the first of its kind in children and the first to provide evidence of these alterations in obese children.
The alterations found in the study are consistent with the changes seen in people with obsessive–compulsive disorder and Prader–Willi syndrome, a genetic disorder that causes obsessive symptoms and leads to obesity. “Obese children suffer greatly from their problem and from the obsessive idea of food,” explained co-author Laura Blanco-Hinojo, a researcher in the Magnetic Resonance Imaging Research Unit. “Moreover, food does not calm them down, they do not enjoy it, and it only partially alleviates their anxiety.” In other words, the obsession with eating invades the mind and the child experiences this negatively and with suffering, which is not the case for normal-weight or overweight children.
The alteration of the behaviour-regulating system can be considered pathological, a fact that must be taken into account when dealing with these cases. “Therapeutic intervention is absolutely necessary and should not be foregone,” explained co-author Gerard Martínez-Vilavella, a psychologist in the Magnetic Resonance Imaging Research Unit at Hospital del Mar. ”In overweight children, there are quantitative alterations that indicate that the brain is functioning differently, but in obese children, it falls into the category of pathology,” he added.
The hyperexcitement of these areas of the brain causes permanent anxiety in obese children and, at the same time, alters and magnifies their perception of their own body. These cases therefore require a multidisciplinary approach, given that the children are still in the process of forming their personality as well as their brain structures and connections.
The researchers noted that the study does not reach a conclusion on whether obesity causes the brain alterations or the alterations cause overweight and obesity. In any case, both factors—diet and brain pathology—must be taken into account. Jordi Sunyer, ISGlobal researcher and last author of the study, commented: “The high prevalence of childhood obesity is one of the biggest epidemics of the 21st century. The discovery of functional alterations in brain regions related to reward and body image in these children indicates that treatment must be targeted at the individual level. The fact that these alterations are also found in brain diseases and mental illnesses provides a clue as to what sort of therapeutic practices are necessary. However, the widespread availability of high-calorie food, excessive screen time and indoor life, and passive mobility are environmental determinants that must also be addressed.”
Childhood obesity
In Catalonia, 38% of girls and 40% of boys aged 6-11 years are overweight or obese, according to a study of more than one million children by ISGlobal and the IDIAPJGol Institute. (The study was published inJama Network Open and is available at the following link: https://bit.ly/3vsICaI.) The prevalence of overweight and obesity has fallen overall but has risen in the most deprived urban areas. Childhood obesity is defined as a weight at or above the 95th percentile for the child’s age.
Reference
Jesus Pujol, Laura Blanco-Hinojo, Gerard Martínez-Vilavella, Joan Deus, Víctor Pérez-Sola, Jordi Sunyer, Dysfunctional Brain Reward System in Child Obesity, Cerebral Cortex, 2021; bhab092, https://doi.org/10.1093/cercor/bhab092